The great divide: How different Covid-19 control strategies shaped pandemic outcomes

By Matt Boyd, Michael Baker, Amanda Kvalsvig & Nick Wilson (cross-posted from the PHCC Blog)

Summary/TLDR
- At the onset of the Covid-19 pandemic, countries responded in a range of ways.
- Our new research reveals that those that put in place explicit exclusion/elimination strategies achieved dramatically lower Covid-19 mortality during the critical 2020-21 period.
- These jurisdictions recorded negative excess mortality—fewer deaths than expected based on previous years—with -2.1 deaths per 100,000 population, compared with 166.5 per 100,000 in other jurisdictions.
- In particular, island jurisdictions with stringent border restrictions experienced substantially better outcomes than non-islands.
- Crucially, we found no consistent evidence that stringent border restrictions harmed economic growth compared to jurisdictions with less stringent restrictions.
- This finding challenges widespread assumptions about inevitable trade-offs between health and the economy.
The strategic divide in pandemic response
Five years into the Covid-19 pandemic, with an estimated 27.3 million excess deaths globally,1 we now can look back and try to understand which control strategies worked best. This question is important, as the world will face more pandemics in the future, possibly even bioengineered ones.2
There are clear strategic choices around how to manage a pandemic. A mitigation/suppression approach accepts ongoing community spread while aiming to slow transmission. An exclusion/elimination strategy aims to prevent or rapidly eliminate community transmission.3
Our new peer-reviewed paper published in PLOS Global Public Health,4 identified five jurisdictions that explicitly pursued exclusion/elimination strategies: Australia, China, New Zealand, Singapore, and Taiwan. These weren’t just jurisdictions with low case numbers—they had exclusion/elimination goals and designed comprehensive policies and programmes around them.
Border restrictions
Central to exclusion/elimination strategies were stringent border restrictions. We analysed when jurisdictions reached maximum border closure (Oxford Stringency Index Level 4) and for how long they maintained these controls. Most jurisdictions (82.8%) eventually reached Level 4 restrictions, but the duration varied dramatically. Oceania maintained the longest median duration (768 days), while Western Europe had the shortest.
Very different health outcomes
The excess mortality differences through 2020–2021 were stark:
Explicit exclusion/elimination jurisdictions:
- Mean age-standardised cumulative excess mortality: -2.1 per 100,000 (negative excess mortality)
All other jurisdictions:
- Mean age-standardised cumulative excess mortality: 166.5 per 100,000

Island jurisdictions overall experienced much lower mortality (64.8 per 100,000) compared to non-islands (194.3 per 100,000), regardless of strategic approach.
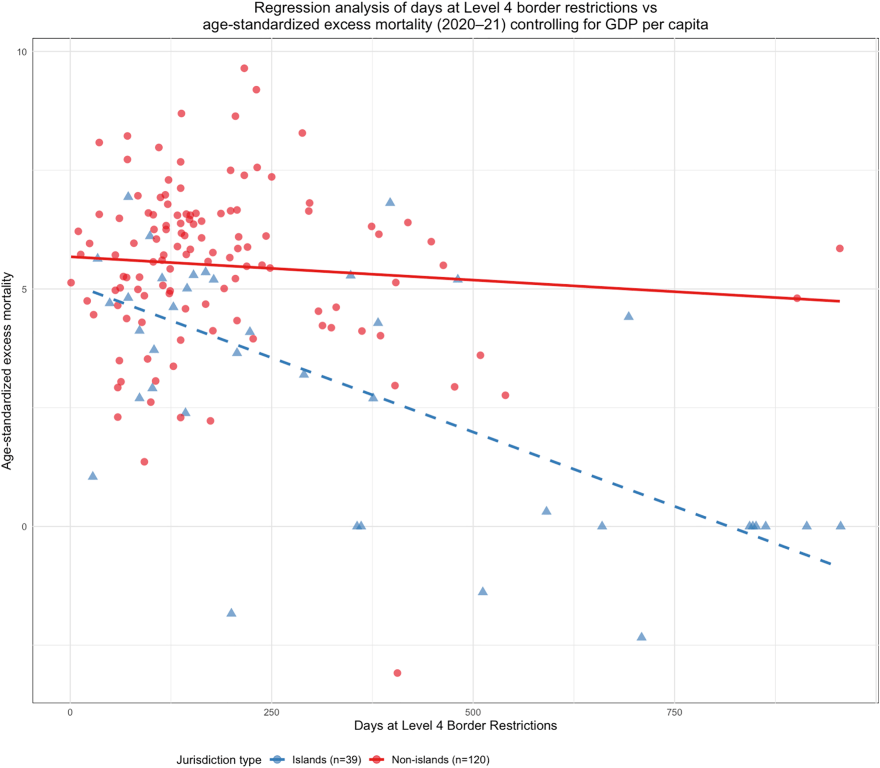
Among jurisdictions implementing Level 4 border restrictions, we found powerful correlations between restriction duration and reduced mortality—but only for islands. That is, in island jurisdictions, the longer border restrictions were in place, the lower the excess deaths. In our regression model accounting for GDP per capita and border restriction duration, these two factors alone explained approximately 58% of the variance in these mortality outcomes (with border restriction duration showing a stronger statistical association with mortality than GDP).
Governance quality: A critical factor
When we controlled for government corruption in our analysis, the picture became more nuanced. The protective effect of border restrictions weakened considerably, while low government corruption itself emerged as a significant predictor of better mortality outcomes.
This finding suggests that effective governance quality, not just border measures alone, was crucial for successful pandemic control. Better-governed jurisdictions (especially the absence of corruption) were more effective at implementing comprehensive public health responses beyond just border restrictions.
Economic impact findings challenge conventional wisdom
One of our most important findings challenges widespread assumptions about health-economy trade-offs. Despite extensive analysis, we found no consistent statistically significant relationships between border measures and GDP growth during the 2020–2021 pandemic period.
The absence of clear economic disadvantages suggests that stringent border restrictions during severe pandemics may not significantly harm economies, relative to those jurisdictions that take other approaches, as is widely assumed.
Seven success stories
Our paper reports on seven jurisdictions that achieved negative age-standardised cumulative excess mortality during 2020–2021, meaning fewer people died than would be expected in normal times. Six were islands (Antigua and Barbuda, Barbados, Iceland, Japan, New Zealand, Taiwan) plus Mongolia. All used quarantine for arrivals and most implemented Level 4 border restrictions, demonstrating that exceptional outcomes were achievable beyond just explicit exclusion/elimination jurisdictions.
Conclusions
The Covid-19 pandemic created a natural experiment in control strategies across the 193 jurisdictions studied. The results suggest that exclusion/elimination approaches, particularly when implemented with strong governance, achieved dramatically superior health outcomes without apparent economic penalties.
Conclusions of this study are consistent with other quantitative evaluations of the health impact of the elimination strategy. A comparison of OECD island countries found that those that had followed the most proactive exclusion/elimination strategy (NZ and Australia) had the lowest excess mortality.5 They also had relatively good macroeconomic performance compared with countries pursuing a suppression strategy. Previous research also confirms NZ had negative excess mortality during the 2020-21 elimination period.6
As we prepare for future pandemic threats, these insights can inform more proactive approaches. While geography provides some countries with natural advantages, governance quality looks to be an important and modifiable factor in determining pandemic response success. For severe infectious disease threats, the evidence increasingly suggests that exclusion and elimination, rather than acceptance and mitigation, is the path to both better health and economic outcomes.
These findings have implications for NZ as the Royal Commission of inquiry Phase Two prepares to submit its report in February 2026 and the Government then needs to formulate its response.7 They are also relevant to informing global pandemic preparedness approaches led by the World Health Organization.8
What this briefing adds
- Jurisdictions implementing explicit exclusion/elimination strategies achieved negative cumulative excess mortality through 2020–21 (-2.1 per 100,000) compared to others (166.5 per 100,000), representing the clearest evidence of the impact of a strategic approach on pandemic outcomes.
- Duration of maximum border restrictions strongly predicted lower mortality in island jurisdictions, but this effect may be partially due to governance quality rather than border measures alone.
- No consistent relationships emerged between stringent border measures and GDP growth, challenging assumptions about inevitable health-economy trade-offs.
Implications for policy and practice
- Future pandemic preparedness should prioritise exclusion/elimination strategies for more severe threats, where geographically and governmentally feasible, particularly for island jurisdictions and countries with strong institutional capacity.
- Investment in governance quality may be as important as specific pandemic policies, since response effectiveness depends heavily on successful implementation.
- Further work is needed to extend and validate this research, including: refining the pandemic response classification of specific jurisdictions; extending the analysis of well-being and economic factors beyond the first two pandemic years; and investigating the role of governance factors.
References
- Mathieu E, Ritchie H, Rodés-Guirao L, et al. (2020) – “COVID-19 Pandemic” Published online at OurWorldinData.org. Retrieved from: https://ourworldindata.org/coronavirus [Online Resource]
- RAND. Global Catastrophic Risk Assessment. Homeland Security Operational Analysis Center; 2024
- Baker MG, Wilson N, Blakely T. Elimination could be the optimal response strategy for covid-19 and other emerging pandemic diseases. BMJ. 2020 Dec 22;371. https://doi.org/10.1136/bmj.m4907
- Boyd M, Baker MG, Kvalsvig A, Wilson N. Impact of Covid-19 Control Strategies on Health and GDP Growth Outcomes in 193 Sovereign Jurisdictions. PLOS Global Public Health. 2025; 5(10) https://doi.org/10.1371/journal.pgph.0004554
- Summers JA, Kerr J, Grout L, et al. A proactive Covid-19 response associated with better health and economic outcomes for OECD High-Income Island Countries. SSM – Population Health 2025;31:101827. https://www.sciencedirect.com/science/article/pii/S2352827325000813
- Plank MJ, Senanayake P, Lyon R. Estimating excess mortality during the Covid-19 pandemic in Aotearoa New Zealand. International Journal of Epidemiology. 2025 Aug;54(4):dyaf093. https://doi.org/10.1016/j.ssmph.2025.101827
- Baker M, Broadbent A, Kvalsvig A, Wilson N. Improving our pandemic preparedness: Counterfactuals and continuous quality improvement. Public Health Expert Briefing. 2025 Apr 16. https://www.phcc.org.nz/briefing/improving-our-pandemic-preparedness-counterfactuals-and-continuous-quality-improvement
- Baker MG, Durrheim D, Hsu LY, Wilson N. COVID-19 and other pandemics require a coherent response strategy. Lancet. 2023 Jan 28;401(10373):265-6 https://doi.org/10.1016/S0140-6736(22)02489-8